8+ Sample Soap Assessment
-
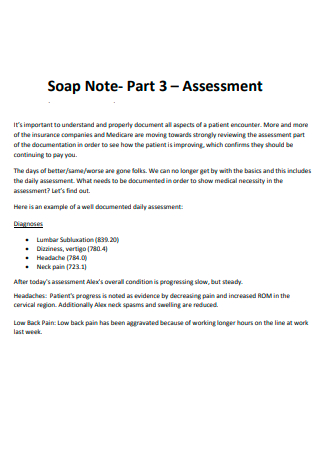
Soap Note Assessment
download now -

Soap Opera Performance Assessment
download now -

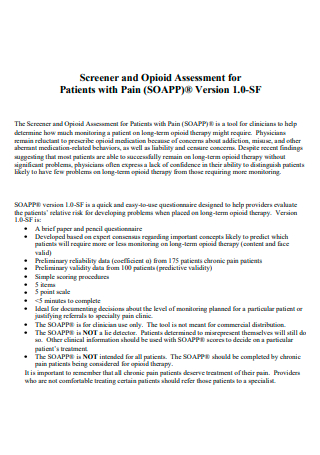
Soap Production Assessment
download now -
Soap Assessment in PDF
download now -

Soap Performance Assessment
download now -
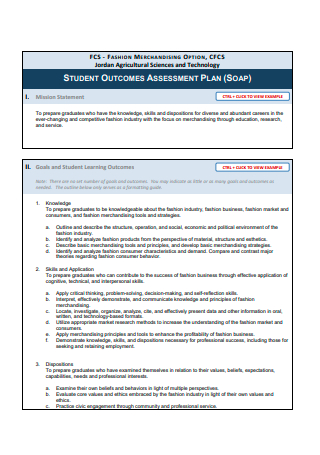
Soap Assessment Plan
download now -
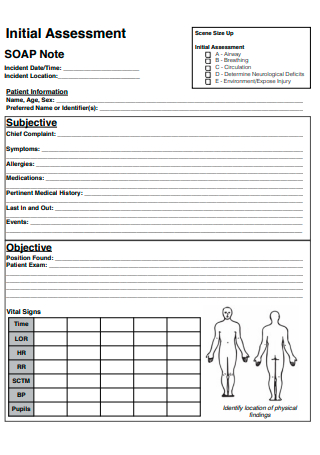
Soap Note Initial Assessment
download now -

Soap Assessment Panel
download now -
Childrens Soap Critical Assessment
download now
FREE SOAP Assessment s to Download
8+ Sample Soap Assessment
What is a SOAP Assessment?
Types of SOAP Assessments
Basic Elements of SOAP Assessment Note
How to Document a SOAP Assessment
FAQs
What should be included in the SOAP note assessment?
What are the basic elements of a SOAP note?
What is the importance of writing SOAP notes?
What is a SOAP Assessment?
A SOAP assessment is a comprehensive method used by many professionals in various industries such as education, mental health, occupational therapy, physical therapy, social work, nursing, and many others to analyze and document every individual encounter to preserve the event for future reference, as well as in accounting and legal purposes. It includes the SOAP note, an intake progress note and a documentation plan for outpatients, medical historical records, physical examination, assessments of various diagnoses, and investigative treatment plans. This is documented in the format of subjective, objective, assessment, and plan which is the pattern integrated for daily inpatient encounters such as comprehensive physical exams and other medical evaluations.
SOAP assessments enable medical practitioners to record a synthesis of subjective and objective evidence to give an in-depth diagnosis and assess the patient’s progress through a standardized analysis of the issue, potential interaction, and status changes. Additionally, it provides accurate information regarding the medical treatment plan, especially on how the patient is responding to the treatment, and the progress or improvements made by the patient. Thus, a SOAP assessment contains medical diagnoses, patient progress, and medication or treatment plan changes.
Types of SOAP Assessments
There are a wide variety of SOAP assessments used by many educators, doctors, nurses, physical therapists, and other medical professionals in different clinical fields. Here are some common types of SOAP assessments.
Basic Elements of SOAP Assessment Note
Assessments using SOAP notes are essential to help medical practitioners to create medical reports and effective treatment plans for their patients, as well as a healthcare operational plan. In this section, learn about the basic elements and structure of a SOAP assessment note.
How to Document a SOAP Assessment
After knowing the basic elements of a SOAP assessment note, you need to follow the basic SOAP framework to help you structure your documentation properly in a consistent manner. Keep it clear and organized while writing the essential details of the assessment.
Step 1. Write the Subjective Section
When you write this section, indicate how the patient is currently feeling and how they have been since the last medical review in their own words. Ask your patient some questions: How are you today? How have you been since the last office visit? Have you currently got any difficult symptoms? Explore each of the multiple symptoms mentioned by the patient and describe them in their own words. Write down the patient’s responses accurately and use quotation marks to directly quote what the patient has stated.
Step 2. Record the Objective Observations
Include in the objective section your objective observations or the things you can see, measure, hear, feel, or smell such as the appearance, clinical examination findings, fluid balance, vital signs, and other medical investigation results. Describe the appearance of the patient, and record the patient’s vital signs such as blood pressure, pulse rate, respiratory rate, and temperature. Include an assessment of the patient’s fluid intake and output such as oral fluids, intravenous fluids, nasogastric fluids or feed, urine output, vomiting, and drain output.
Step 3. Detail the Assessment
Document your thoughts on the clinical diagnosis and the salient issues based on the gathered information in the previous sections. Summarise the salient points (e.g., “Increasing shortness of breath”, “Raised white cell count (15) and CRP (80)”, “Chest X-ray revealed increased opacity in the right lower zone, consistent with consolidation”, etc.) Write down your impression of the diagnosis. If it is an already-known diagnosis, include comments on whether the patient is clinically improving or deteriorating.
Step 4. Outline the Plan
Develop a treatment plan on how you will address or further investigate any problems raised during the clinical review. Incorporate in your plan some necessary items such as more medical investigations like laboratory tests and imaging, medical treatments such as nutrition, medications, intravenous fluids, and oxygen, referrals to specific specialties, time and date of review, frequency of observations and monitoring of fluid balance, and planned discharge date.
FAQs
The SOAP note assessment should include your major observations from the assessment which are the things you can measure like the vital signs, fluid balance, clinical examination findings, and investigation results. Record the patient’s vital signs such as blood pressure, pulse rate, respiratory rate, SpO2 (supplement oxygen), and body temperature. When assessing the patient’s fluid intake, you must include the output of the patient such as the nasogastric fluids, intravenous fluids, drain output/stoma output, oral fluids, intravenous fluids, urine output, and vomiting. Some medical investigation result examples that you may add are recent lab results like blood tests and imaging results like chest X-rays.
What should be included in the SOAP note assessment?
The basic elements of a SOAP note are subjective, objective, assessment, and plan.
What are the basic elements of a SOAP note?
Writing SOAP notes is important for academic professionals and medical specialists to document what they accomplished and observed to help them track the results, scores, or goals in the assessment.
What is the importance of writing SOAP notes?
It is integral to document and explain the core points of SOAP assessment work in various fields and industries such as education, mental health, physical therapy, and other medical fields. Take note of the different SOAP assessments, the basic elements of a SOAP assessment note, and the basic steps to document a SOAP assessment for your patients. Thus, here are some of our sample downloadable and printable SOAP assessment document templates available in PDF format. Browse and use the sample SOAP assessments and other assessment forms available on Sample.net such as a client biophysical assessment and a project assessment plan.
