8+ Sample DAP Notes
-
DAP Therapist Confidential Note
download now -
Sample DAP Notes
download now -
DAP Progree Notes
download now -

SOAP and DAP Note
download now -
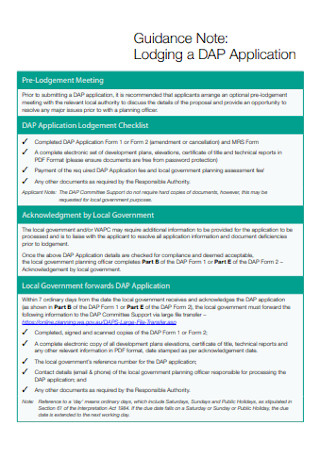
Lodging a DAP Application Note
download now -
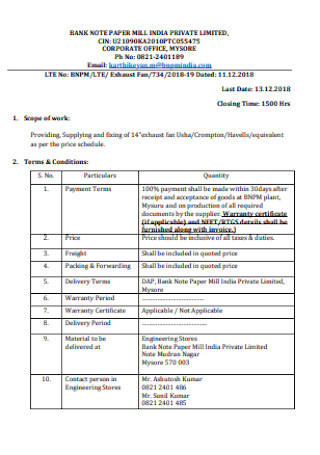
DAP Bank Note
download now -
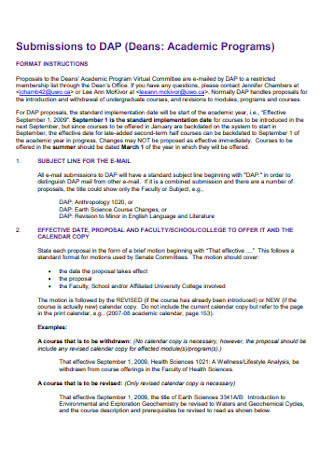
Submissions to DAP Note
download now -

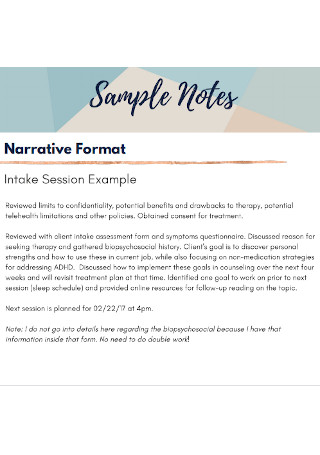
Sample Progress Note
download now -
DAP Note Format
download now
FREE DAP Note s to Download
8+ Sample DAP Notes
What Is a DAP Note?
Definition of Acronyms
Areas Where DAP Notes are Commonly Used
Skills Needed in Taking Down DAP Notes
Uses of DAP Notes
Do’s in Writing DAP Notes
Don’ts of Writing DAP Notes
How to Write DAP Notes
FAQs
What does DAP stand for in counseling notes?
How do you write progress notes faster?
How do you write a good DAP note?
How long should a DAP note be?
What is the difference between SOAP and DAP?
What does a DAP note look like?
What Is a DAP Note?
DAP notes are short notes that are typically used by professionals in the field of healthcare and behaviora chart sciences. DAP stands for data, assessment, and plan.
According to an online article published by GoodTherapy, DAP is only one approach used by clinicians and psychologists. The DAP and SOAP formats are commonly used as templates for progress notes in the field of psychotherapy. Similar to DAP notes, SOAP means subjective statement, objective data, assessment, and plan.
Definition of Acronyms
D– The D stands for data. This is a narration of what transpired during a meeting. And it includes everything that is observable. What can be initially observed from the clients through client list as soon as they walk through the door or sit down? It can be their appearance, words they uttered, feelings they shared, and even body language. Essentially, your data is anything that was said and done during the meeting or session.
A– The A stands for assessment. The professional taking down the notes then proceeds to assess the data he or she has gathered from the patient. This entails listing down hypotheses and other professional interpretations. For instance, a therapist deduces from his initial observations that a patient is preoccupied or anxious because she is constantly checking her phone or the wall clock. The assessment is basically a tool for you to judge how you understand the situation, why the patient may be feeling or acting this way, etc.
P– The P stands for plan. After the professional assessment report, conclude the notes by creating a follow up plan. It usually involves scheduling the next session and determining the topics to be covered next. As a response to the assessment, a professional may prescribe treatment, refer the patient to another agency, choose to continue or discontinue any medication, continue with the sessions, or make modifications to the program.
Areas Where DAP Notes are Commonly Used
DAP notes are normally used in the field of behavioral science. The following fields are some examples:
Skills Needed in Taking Down DAP Notes
Uses of DAP Notes
Do’s in Writing DAP Notes
Don’ts of Writing DAP Notes
How to Write DAP Notes
Keeping the above tips in mind, you can now begin writing your DAP notes. Follow these basic steps:
Step 1: Basic Information
On the top most part of your page, include the patient or client’s name and age. Don’t forget to indicate the date. You can also note the time or length of the session. Recording basic information is needed to ease the documentation process.
Step 2: Data Gathering
Start your notes by writing down all the data you are able to gather from the patient or meeting. These can be both objective and subjective. Objective data are the hard facts that you notice about the situation. Subjective data are based on your initial assumptions and preconceptions about the patient’s mood, feelings, etc.
Step 3: Assessment of Data
What can you establish based on your understanding of the data? You can freely interpret, compare and contrast, and analyze the overall situation and circumstances. What can you deduce about the client’s behavior? What does it all mean and why may that be the case? In the case of trauma patients, a therapist may observe a shift in behavior and create a hypothesis as to why there was an apparent shift. Keep your evaluations concise and professional; while using the right keywords and assigning the appropriate clinical terms.
Step 4: Plan of Action
The last step is the planning stage. Draft a concrete plan and outline the goals for your subsequent meetings. You can include the next steps or agenda of the next session. You can also indicate if the client’s current program should be continued or would need sufficient changes and modification. In the case of a patient undergoing treatment, you may see treatment plan. you can plan whether to maintain the same treatment, change strategies, or stop the treatment altogether.
FAQs
What does DAP stand for in counseling notes?
DAP stands for data, assessment, and plan. In the field of behavioral science, a psychiatrist or psychologist may use this method when counseling patients suffering from mental illnesses, addictions, trauma, etc. The notes are written in chronological order where data is first gathered, assessed, then acted upon in the plan phase.
How do you write progress notes faster?
One technique you can apply is to write down the keywords or main phrases. Try leaving out the unnecessary and trivial information. You need to be able to discern the main points if you want to write your notes faster and keep up with the patient or situation as it unfolds.
How do you write a good DAP note?
A good DAP note is brief, concise, and concrete. Make sure only the relevant details are included. The data should be accurately described and narrated. Your assessment should be clear, insightful, and in-depth. And lastly, your plan should be action-oriented, realistic, and concrete.
How long should a DAP note be?
A good DAP note is brief and straightforward. It should only contain the key ideas and main points; and shouldn’t be longer than a couple of pages. It’s important to organize your notes well so the main ideas are clearly presented and easily identifiable.
What is the difference between SOAP and DAP?
The SOAP and DAP formats are two commonly used templates for progress notes, as far as psychotherapy is concerned. The two approaches are basically the same as they both require data collection, a professional assessment, and a plan of action. The only difference is that the SOAP method breaks down the initial observations into two: subjective statement and objective data.
What does a DAP note look like?
A DAP note can come in any form. It would usually depend on the therapist or researcher who is writing it. It can be in a questionnaire format or a blank, single page document where the therapist just fills in the details.
The DAP method is beneficial in multiple fields. It’s an effective strategy when time is constrained. It helps the therapist or researcher focus on what matters; and gives them a structure to follow when they’re working in the field or talking to a patient. Check out the sample templates above and customize it to suit your needs!
